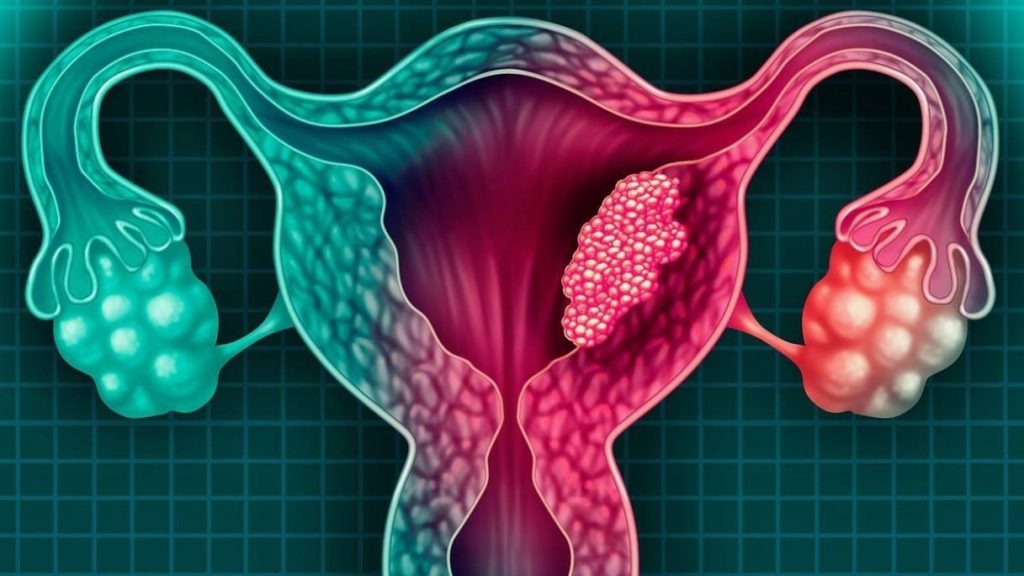
Uterine fibroids, also known as leiomyomas or myomas, are benign, well-circumscribed, encapsulated tumors arising from the smooth muscle cells of the cervix or body of the uterus. These non-cancerous growths are among the most common tumors in the female genital area, affecting approximately 20-40% of women of reproductive age. Fibroids can vary greatly in size, from as small as a pea to as large as a melon, and can be singular or multiple. They can develop in different parts of the uterus and have various effects on a woman’s health depending on their size, number, and location. Treatments for fibroids are often available at specialized medical centers, including aesthetic clinic, which focus on minimally invasive procedures to enhance overall wellness.
Causes of Uterine Fibroids
The exact cause of uterine fibroids remains unknown, but several factors are believed to contribute to their development:
1. Hormonal Factors: Estrogen and progesterone, the hormones that stimulate the development of the uterine lining during each menstrual cycle in preparation for pregnancy, appear to promote the growth of fibroids. These hormones contribute to the fibroids’ growth by increasing the rate of cell division in the smooth muscle cells of the uterus.
2. Genetic Predisposition: Women with a family history of fibroids are more likely to develop them. Genetic mutations in the cells of the smooth muscle of the uterus can lead to the growth of fibroids.
3. Age: Fibroids are most common in women in their 30s and 40s through menopause. After menopause, fibroids usually shrink due to a decrease in hormone levels.
4. Ethnicity: African-American women are more likely to develop fibroids and at a younger age than women of other ethnic groups. They also tend to have more severe symptoms and larger fibroids.
5. Lifestyle Factors: Obesity, a diet high in red meat and low in green vegetables, fruit, and dairy, as well as alcohol consumption, can increase the risk of developing fibroids. Additionally, lack of physical activity and stress may contribute to fibroid growth.
6. Reproductive History: Women who have never given birth are at higher risk of developing fibroids.
Clinical and Anatomical Classification
Uterine fibroids can be classified based on their location within the uterus:
1. Intramural Fibroids: Located within the muscular wall of the uterus, these are the most common type. They can cause the uterus to appear larger than normal, potentially affecting its function.
2. Submucosal Fibroids: Protrude into the uterine cavity, often causing heavy menstrual bleeding and other more severe symptoms. These fibroids can distort the uterine cavity and interfere with fertility.
3. Subserosal Fibroids: Extend beyond the wall of the uterus into the pelvic cavity, sometimes becoming pedunculated (attached to the uterus by a thin stalk). They can cause pressure on surrounding organs such as the bladder and rectum.
4. Cervical Fibroids: Develop in the cervical tissue, which can lead to complications during childbirth and affect the function of the cervix.
Clinical Manifestations
The symptoms of uterine fibroids can vary widely, depending on their size, number, and location. Common clinical manifestations include:
1. Menstrual Changes: Heavy and prolonged menstrual periods, sometimes with clots. Menstrual bleeding may be so severe that it leads to anemia and the need for medical treatment.
2. Pelvic Pain and Pressure: Chronic pelvic pain, pressure, or a feeling of fullness in the lower abdomen. Pain can be localized to specific areas and may worsen during menstruation.
3. Reproductive Issues: Infertility, miscarriage, and complications during pregnancy and labor. Fibroids can interfere with the implantation of the embryo and cause pregnancy loss.
4. Bladder Problems: Frequent urination or difficulty emptying the bladder due to pressure on the bladder. In severe cases, urinary retention and kidney damage can occur.
5. Bowel Issues: Constipation and bloating due to pressure on the rectum. Large fibroids can obstruct the bowel, leading to significant discomfort and digestive problems.
6. Lower Back Pain: Pain that radiates to the lower back and legs due to pressure on nerves.
7. Painful Intercourse: Discomfort or pain during sexual activity, especially with certain positions.

How Fibroids Affect the Body
Fibroids can significantly impact a woman’s quality of life by causing discomfort, pain, and a variety of other symptoms. In severe cases, fibroids can lead to complications such as:
1. Anemia: Due to heavy menstrual bleeding, leading to fatigue, weakness, and other health issues.
2. Infertility: By interfering with the implantation of a fertilized egg and causing structural abnormalities in the uterus.
3. Pregnancy Complications: Including preterm birth, breech birth, and the need for a cesarean section. Fibroids can also increase the risk of placental abruption and postpartum hemorrhage.
4. Urinary Problems: Due to pressure on the bladder, leading to frequent urination, urgency, and, in severe cases, urinary retention.
5. Bowel Obstruction: Large fibroids can press against the rectum, causing constipation and bowel obstruction.
6. Hydronephrosis: Swelling of the kidneys due to obstruction of the urinary tract caused by large fibroids.
7. Impact on Sexual Health: Fibroids can cause painful intercourse and decrease sexual satisfaction.
Diagnostics
Diagnosing uterine fibroids typically involves:
1. Pelvic Examination: To check for irregularities in the shape of the uterus. A gynecologist may feel for an enlarged or irregularly shaped uterus during a routine pelvic exam.
2. Ultrasound: To visualize the fibroids and determine their size and location. Both transabdominal and transvaginal ultrasounds may be used to get detailed images of the uterus.
3. Magnetic Resonance Imaging (MRI): Provides detailed images of fibroids and helps in planning treatment, especially for larger or multiple fibroids.
4. Hysterosonography: Uses saline to expand the uterine cavity for better imaging of submucosal fibroids.
5. Hysteroscopy: Involves inserting a small, lighted telescope through the cervix to examine the inside of the uterus. This procedure can also be used to remove small fibroids.
6. Laparoscopy: A minimally invasive surgical procedure where a small camera is inserted through a small incision in the abdomen to view the outside of the uterus and other pelvic organs.
Treatment
Treatment options for uterine fibroids depend on the severity of symptoms, the size and location of the fibroids, and the patient’s desire for future pregnancies:
1. Medications:
– Hormonal Therapies: Gonadotropin-releasing hormone (GnRH) agonists can shrink fibroids by decreasing estrogen and progesterone levels. Birth control pills can help control heavy bleeding.
– Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can relieve pain associated with fibroids.
– Iron Supplements: To treat anemia caused by heavy menstrual bleeding.
2. Non-Invasive Procedures:
– MRI-guided Focused Ultrasound Surgery (FUS): Uses high-intensity ultrasound waves to destroy fibroid tissue without damaging surrounding tissues.
3. Minimally Invasive Procedures:
– Uterine Artery Embolization (UAE): Blocks the blood supply to fibroids, causing them to shrink.
– Laparoscopic or Robotic Myomectomy: Removal of fibroids through small incisions using specialized instruments.
– Hysteroscopic Myomectomy: Removal of submucosal fibroids using a hysteroscope inserted through the cervix.
4. Traditional Surgical Procedures:
– Abdominal Myomectomy: Surgical removal of fibroids through an abdominal incision.
– Hysterectomy: Complete removal of the uterus, which can be performed via the abdomen, vagina, or using laparoscopic methods. This is a definitive cure for fibroids but results in the loss of fertility.
Types of Operations for Uterine Fibroids
1. Myomectomy: Surgical removal of fibroids while preserving the uterus.
– Hysteroscopic Myomectomy: For fibroids inside the uterine cavity, performed using a hysteroscope.
– Laparoscopic Myomectomy: For fibroids on the outer surface or within the wall of the uterus, performed using small incisions and a laparoscope.
– Abdominal Myomectomy: For larger or more numerous fibroids, performed through an open abdominal incision.
2. Hysterectomy: Complete removal of the uterus, which can be performed via different approaches:
– Abdominal Hysterectomy: Removal of the uterus through an incision in the abdomen.
– Vaginal Hysterectomy: Removal of the uterus through the vagina.
– Laparoscopic Hysterectomy: Removal of the uterus using a laparoscope and small incisions.
Complications
1. Severe Anemia: Due to heavy bleeding, leading to fatigue, weakness, and other health issues.
2. Acute Pain: From fibroid degeneration or torsion, causing severe abdominal pain and requiring immediate medical attention.
3. Infertility: Fibroids can interfere with implantation and pregnancy, causing difficulty in conceiving.
4. Impact on Pregnancy: Increased risk of cesarean section, preterm delivery, and breech birth. Fibroids can also increase the risk of placental abruption and postpartum hemorrhage.
5. Hydronephrosis: Swelling of the kidneys due to obstruction of the urinary tract caused by large fibroids.
6. Bowel Obstruction: Large fibroids can press against the rectum, causing constipation and bowel obstruction.
Prevention of Uterine Fibroids
While it is not always possible to prevent fibroids, certain lifestyle changes may help reduce the risk. The following ways can help prevent it.
1. Healthy Diet: Emphasize fruits, vegetables, and low-fat dairy products while reducing red meat consumption. A diet rich in green vegetables and fruits can help balance hormone levels and reduce the risk of fibroid growth.
2. Regular Exercise: Helps maintain a healthy weight and reduce hormone levels that can stimulate fibroid growth. Physical activity also helps in managing stress, which can contribute to hormonal imbalances.
3. Weight Management: Maintaining a healthy weight can reduce the risk of developing fibroids, as excess body fat can produce estrogen.
4. Regular Medical Check-ups: Early detection and management of fibroids can prevent complications. Regular pelvic exams and ultrasounds can help monitor fibroid growth and manage symptoms effectively.
5. Stress Management: Reducing stress through relaxation techniques, yoga, and other stress-relieving activities can help maintain hormonal balance.
Importance of Contacting Trusted Clinics
Given the complexities associated with diagnosing and treating uterine fibroids, it is crucial to consult with reputable healthcare providers. Trusted clinics offer access to experienced specialists, advanced diagnostic tools, and a wide range of treatment options tailored to the patient’s specific needs. Early intervention and appropriate management can significantly improve outcomes and quality of life for women with fibroids.
Factors to Consider
1. Reputation: Look for clinics with a strong reputation and positive patient reviews.
2. Specialization: Ensure the clinic has specialists in gynecology and fibroid treatment.
3. Technological Capabilities: Advanced diagnostic and treatment options, such as MRI-guided focused ultrasound surgery and minimally invasive procedures.
4. Comprehensive Care: Clinics that offer a multidisciplinary approach, including medical, surgical, and supportive care.
End Note
In conclusion, while uterine fibroids are common and often benign, they can cause significant discomfort and complications for many women. Understanding the causes, symptoms, diagnostic methods, and treatment options is essential for managing this condition effectively. Regular consultations with healthcare professionals and adopting a healthy lifestyle can help mitigate the impact of fibroids and enhance overall well-being.

I like to give reasonable advice on budgeting to people with any income level. I currently live in Portland, Oregon, and am available for freelance assignments and speaking engagements.
